Why parents get into counterproductive feeding patterns: Worry Cycle Part II
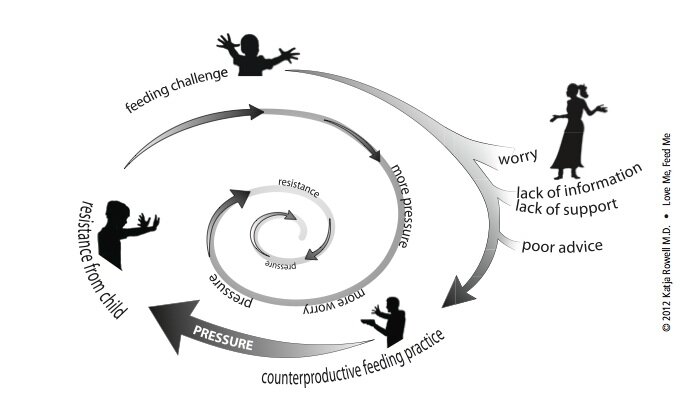 Last week's post introduced the "Worry Cycle" and why some foster and adopted children present with feeding challenges. The child who is challenging to feed is often the starting point that sets up the difficult feeding relationship.This week we move on to the parent dealing with the feeding challenge. Obviously, this is where I want to break the cycle, by offering information and support about best-feeding practices, even in the face of significant challenges...
Last week's post introduced the "Worry Cycle" and why some foster and adopted children present with feeding challenges. The child who is challenging to feed is often the starting point that sets up the difficult feeding relationship.This week we move on to the parent dealing with the feeding challenge. Obviously, this is where I want to break the cycle, by offering information and support about best-feeding practices, even in the face of significant challenges...
Poor support
One mom said that "beyond bottle feeding" there was little information out there about how important feeding was for her foster children. Another mother said that beyond being told to give their son a food stash, they had no real guidance about how her adopted son's history of food scarcity would play out. (See my guest post on food hoarding and integrating a child into a family's food culture at Fostering Thrifty Families.)“Despite having read a TON in preparation, I wish I had known how much feeding is a key for attachment, even for older children. I wish I had had more information that there was a good chance that the table could be a very difficult place for a while, and some of the reasons for that—that is, the possibilities of chewing/swallowing/sensory issues. I may have been better able to stay calm and let some things slide if my expectations of a happy family meal had not been met with such a slap in the face.”
Poor advice
From mothers, mothers-in-law, friends, phone apps, to local news, bad feeding advice abounds:
"Just make him eat it!" "No kid starved himself, just serve green beans until he eats. " "I fed you rice cereal when you were two weeks old, she'll be fine!" "Your daughter will be fine, even if she doesn't eat a thing for three weeks." (From a pediatrician!)
Perhaps the most vexing and tragic aspect of the work I have been doing with families is that the lack of support and poor advice often comes from the very experts parents turn to for help: doctors are putting food insecure children on diets, speech therapists are force-feeding children or recommending parents withhold attention and love to get a child to eat...*And here is where I let you in on a dirty little secret. Even though one in three parents will talk to their child's doctor about a feeding concern, doctors almost universally get no training in assessing or addressing feeding and growth issues. I didn't. It's just not in the curriculum. I went to a top ten medical school, and I had no information on feeding issues. I went to a well-respected primary care residency program where I got no training. Yet, I felt I was qualified to give feeding advice. Looking back now, I know I wasn't trained to do so. The ignorance continues. When I've done workshops with pediatrics and FP residents, they still aren't getting any of this info, even though 80% of children with special needs will struggle with feeding, and an estimated 20% of children are felt to have a "feeding disorder." I've also given workshops to feeding therapists who aren't aware of feeding research, the Division of Responsibility, or the responsive feeding literature... (Chapter 3 goes into more detail on feeding therapies and finding the right help for your challenges...)
Worry Fuels Counterproductive Feeding
Why does it matter so much that parents aren't adequately prepared and are given poor advice? Because it fuels the worry, and parents to try to figure it out on their own, or advice leads directly to the counterproductive feeding practice. Parents are already worried and want to do the right thing. When you then have a doctor telling you your child is "obese" or "overeating" and has to be controlled and put on a diet, parents do as they are told, with predictable results. If a pediatrician tells a desperate parent to "do whatever you have to to get food into that child," is it then a surprise when that parent holds the infant's head down to get formula in, or screams and threatens the older child to eat? Misunderstandings about growth, feeding research, and how a child's history plays a role, lead loving and worried parents to pressure with feeding, and that pressure almost never helps..."My child is too small, my child is too big, my child doesn't get enough DHA or protein, my child gets too much sugar..." All of these worries lead parents to feed with an goal: to get the child to eat more, or less, or different kinds of foods. This agenda is at the bottom of the pressure and pushing with feeding.Next we will examine what that pressure looks like. What are counterproductive feeding practices? Sure, we can all agree that holding a child's head down to eat won't help, but even sticker charts and praise can turn some children off. Tune in next week.(Perhaps I should have added the parent's own issues and history around food at this point. If the parent has a history of an eating disorder or has been yo-yo dieting for years, or himself has a history of food insecurity, trusting this process will be even harder...)
* "Questionable things experts say" series: #1 (random sampling), and #2 (do whatever you have to to get that kid to eat) and #3 (stop breastfeeding your "obese" infant at night) and #4 (douse it in ranch) and #5 (just don't bring it into the house). Can you add others?
Note, this is a brief introduction to complex feeding challenges. For more detail, read Love Me, Feed Me: An Adoptive Parent's Guide to Ending the Worry About Weight, Picky Eating, Power Struggles and More. For every book sold for November, National Adoption Month, I will donate $1 to the SPOON Foundation.
